Pithiatism Redux
0 View
Share this Video
- Publish Date:
- 26 February, 2022
- Category:
- Natural Cures
- Video License
- Standard License
- Imported From:
- Youtube
Tags
BY MARTIN SAMUELS
Those of us in medicine have all seen the famous painting of the Tuesday afternoon lessons at the Salpȇtrière in Paris in the 19th century. In Pierre Aristide André Brouillet’s painting, one can clearly see the great professor, Jean-Martin Charcot, holding forth while the patient, Blanche Whitman, is being supported by a tall young man, Joseph Jules Francois Felix Babinski, the Chef de Clinique (the chief resident) and allegedly the favorite to succeed Charcot. He never did as he was failed repeatedly on the exam necessary to become a faculty member at the university by a jealous, xenophobic, anti-immigrant rival, Charles Bouchard. Babinski was born in France and served in the army twice, but his name was Polish as his parents had emigrated to France to escape bias in Poland (sound familiar?). Ironically almost no one remembers Bouchard (his only contribution being the Charcot-Bouchard aneurysm which may be the cause of some intracerebral hemorrhages), but there is no doctor on earth who does not know Babinski’s name. This is one of many reasons why Babinski is my neurological hero.
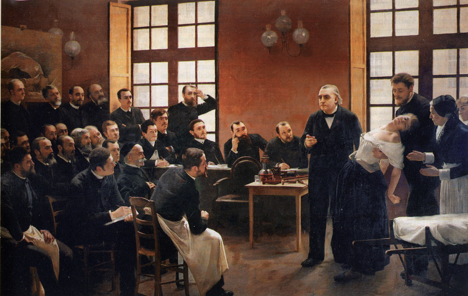
A Clinical Lesson at the Salpêtrière, Pierre Aristide Andé Brouillet
Charcot was a master of the clinical-pathological method whereby he was able to recognize and describe such disorders as amyotrophic lateral sclerosis and multiple sclerosis. In the twilight of his career, Charcot became obsessed with what at the time was called hysteria. He applied his tried-and-true clinical-pathological methods searching for the lesion in the nervous system causing the array of disorders that fell under the rubric of hysteria. These included both attacks of neurological symptoms (eg paralysis, blindness, seizures, loss of sensation, gait disorders, and coma) and a way of life characterized by bouts of illness, fatigue, and weakness (neurasthenia). The Salpȇtrière was an old hospital converted from a gun powder factory (hence the name saltpeter) that was more than a hospital. It was a safe haven for homeless women. Thus Charcot, trapped by acquisition bias, believed that hysteria was a disease of women (hence the reference to the uterus that was first suggested by the Greek school of ) and that it could be treated by various manipulations of the uterus and ovaries and also hypnosis. Charcot died having never found the lesion in the nervous system responsible for this illness. After Charcot’s death, Babinski revealed his longstanding skepticism of the concept of hysteria. He suspected that the dramatic “shows” that were performed at the famous Tuesday afternoon sessions actually reflected a usually unconscious folie a deux between the patient and the professor. By participating in these demonstrations some patients, Charcot’s muses, such as Blanche Whitman, became famous and were the recipients of better living conditions in the Salpȇtrière. It was a Catch 22. One had to be crazy to get better. Whether these muses were “consciously” cooperating with Charcot, for both of their benefits, is undeterminable as it begs the question of will, which is a conundrum that interferes with the proper care of patients. It is always best to start by believing the patient. Willful deceit (i.e. malingering) does, of course, exist, but it is best practice to only resort to that explanation when all other possibilities are excluded. It almost never helps to think that a patient is a copy of the Baron von Munchausen or his pop-culture of The Music Man, the charming sociopath.
Thus Babinski suggested the term pithiatism, which according to my colleague, Marinos Sotiropoulos, was created by combining the Greek words “pitho-” (persuasion, as in Peitho, the mythical Goddess of persuasion) and “-iatos” (curable, an adjective with the same roots as iatros, meaning doctor).
In fact, together with his colleague, Jules Froment, Babinski wrote an entire monograph on the subject, published in 1918 in which they argued that the term was meant to convey that these disorders were caused by suggestion and cured by persuasion by the doctor. “Hysteria is a pathological state manifested by disorders which it is possible to reproduce exactly by suggestion…and can be made to disappear by the influence of persuasion (counter-suggestion) alone.” In the preface by the eminent British Neurologist, E. Farquhar Buzzard, it was suggested that the principles were correct but the term pithiatism might “not be destined for general adoption….there is no doubt that there has been much confusion as to the meaning of hysteria in the mind of the public as well as in that of the medical profession. Perhaps a new name may be associated with a clearer understanding and may escape the obloquy attaching to its predecessor.” That was a prescient suggestion, and now is the time.
After Babinski, the term hysteria was replaced with conversion disorder and dissociative states, based on the influence of another acolyte of Charcot, Sigmund Freud. His concept was that conversion was a form of “body language” whereby a patient acts out an unconscious conflict (converts it), which may also be revealed in surrealistic dreams which could be interpreted to reveal underlying psychological stress. Recall that surrealism was actually born at the Pitié Hospital where Babinski worked as one of his residents was Andre Bréton who wrote that watching Babinski examine a patient was the ecstatic experience that led Breton to leave neurology and found the surrealist movement. This period was followed by the rise of “biological psychiatry” and, with it, the anti-Freud movement which moved “alienism” (the old name for psychiatry) into neuropsychiatry, where the field currently resides. Another irony is that modern functional neuroimaging has produced a new form of Charcot’s clinical-pathological method and the search for the lesion of hysteria goes on today, probably with the same result.
With these changes, a new name for hysteria was coined to help deal with the misogynistic implication of this being a manifestation of “weakness” in females. Babinski violently disagreed with this concept because of his experience in the then all-male military where identical symptoms were rampant. Hysteria was clearly an equal opportunity syndrome, but what to call it to avoid the stigma that psychogenic illness had come to cause? Hence, a “functional” disorder was born. Though innocent-sounding the term is neither accurate nor helpful. Many disorders are functional (e.g. migraine, epilepsy, vasospasm, irritable bowel syndrome) but have no relationship to the disorders from which “hysterical” patients are subject. It also contains no implications for treatment. It is just a euphemism.
It’s time to return to Babinski’s term, pithiatism. It is not judgmental and simply describes the key features of the illness and its treatment: caused by suggestion and cured by persuasion. The suggestion may come from within the patient or from society (via the news or social media). It explains the long history of epidemic illnesses caused by stress, defined by Ivan Pavlov as a life-threatening stressor with no chance of escape or control. Social media have amplified the effect of external stressors (e.g. storms, fires, murders, floods, disease) but the principles remain the same as those seen in the Pitié-Salpȇtrière and during wars. The disorder may, indeed, be more common in women in civil society simply because women are more likely to be placed in stressful circumstances with little chance of escape or control. Babinski’s experience in the army proves that men are just as susceptible if the environment is toxic enough.
In the office, I spend a great deal of time using persuasion to help my patients; a form of modern hypnosis or Mesmerism (focused attention) to relieve suffering using the power of the reflex hammer, the tuning fork, and persuasion by the aged doctor.

Dr. Martin A. Samuels, 2nd from left
Recommended Reading:
Babinski JFF, Froment J. Hysteria or Pithiatism and Reflex Nervous Disorders in the Neurology of War. University of London Press. London. 1918.
Philippon P, Poirier J. Joseph Babinski. Oxford University Press. Oxford and New York. 2009
Hustvedt A. Medical Muses. W.W. Norton & Company. New York and London. 2011.
Martin Samuels is a professor of neurology at Brigham and Women’s Hospital.












