The Courage of Corporate America is Needed to End America’s Opioid Crisis
0 View
Share this Video
- Publish Date:
- 11 December, 2023
- Category:
- Natural Cures
- Video License
- Standard License
- Imported From:
- Youtube
Tags

By RYAN HAMPTON
A Kaiser Family Foundation tracking poll published in July found that three in ten U.S. adults (29%) said they had someone in their family who struggled with opioid dependence. Also surprising, and encouraging, was the statistic that 90% support increasing access to opioid use disorder treatment programs in their communities.
As a person in recovery from opioid use disorder and advocate, my read on this data set is that the public support is there. Now more than ever, we need leaders in healthcare, public policy, and corporate America to have the courage to advance effective treatment options. The most inspiring example of the kind of courage we need was the recent news that one of the nation’s largest retail grocery and pharmacy chains, Albertsons, made the financial investment to train their pharmacy staff to administer buprenorphine injections (known as Sublocade) on site.
To someone who is not in the weeds on the issue of opioid use disorder (OUD) treatment programs, this may just sound like a solid business decision. But go a layer deeper and the courage is evident: Albertsons decided to invest in an underutilized treatment option (despite buprenorphine being the gold-standard in OUD treatment) that serves a highly stigmatized patient population who is often shunned at pharmacy counters nationwide. Albertsons chose to put treatment centers for an underserved and highly stigmatized patient population in the middle of their family-friendly, neighborhood grocery pharmacy chain.
The company rightly recognized that OUD impacts every family and community in this country—including the lives of its patrons. Albertsons pushed through stigma, not leaving the overdose crisis for someone else to address, because it had the ability to provide widespread access through its pharmacies and locations across the nation.
This kind of principled leadership at the corporate level is truly inspiring.
Investing in Solutions is Critical to Ending OUD
It’s easy to say we want to do the right thing, but it takes courage to actually do it. And though many of Albertsons’ customers surely know someone affected by OUD, they (like most people) don’t have a true understanding of the disorder. Without courage, that ignorance will affect our country’s ability to end this health crisis.
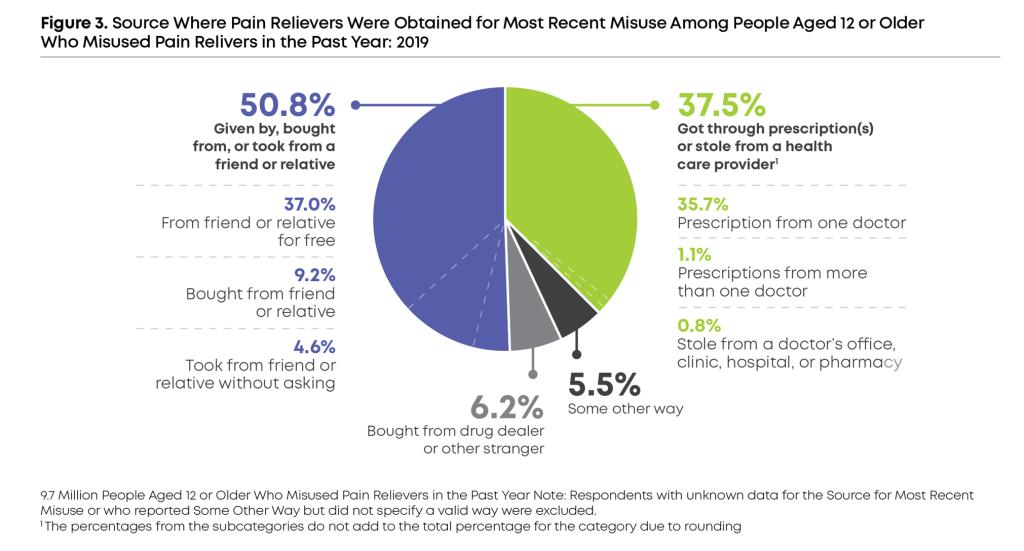
When I talk to people about what I do, most are shocked to learn basic facts about opioid use disorder (OUD). For example, few people know that one-in-three people with OUD were exposed to opioids through a legal prescription for pain from their doctor.
Most assume this problem is isolated to the unhoused and people in custody, when in fact more than half of people are employed, in school or full-time parents. And, sadly, too few people know—including those who suffer from OUD—that the disorder can be treated effectively with medication in an outpatient or virtual setting, for less than $500 a month, including the cost of medication.
When I lay out the facts, that OUD impacts a diverse group of Americans, that there’s an effective and affordable way to treat it that’s accessible on an outpatient basis—the next obvious question is, why aren’t we doing more?
My answer is: we lack courage. Without courage, companies would not mobilize recovery, like Albertsons did, and investors would not back start-ups that are trying to tackle this problem.
For investors, it’s certainly much safer to bet on companies with a clear path to high returns: especially in the healthcare space. We see this all the time when venture capital makes big bets on established players. But people who fund treatment programs that focus on the most vulnerable—and least powerful—in our society exemplify the kind of courage I am talking about.
In recent years, this courage has paid off. Over the last three years, venture capitalists have invested in companies to help scale telehealth treatment programs for OUD—effectively reaching thousands of patients across many states. These programs have impressive, peer-reviewed, clinical outcomes, and these models are repeatable and effective.
The only reason programs like this are not available in all 50 states is because regulators lack the courage to act. Many state and federal regulators who were eager to embrace telehealth during the pandemic have been slow to make these changes permanent, despite the overwhelming evidence that telehealth is an effective way to deliver treatment for OUD, and that traditional treatment programs are not able to meet the needs of all patients.
Certainly, office-based opioid treatment (OBOT) programs have a role to play in addressing the crisis, but they can’t do it alone. This fact was on full display in states like Alabama and Michigan over the last few years.
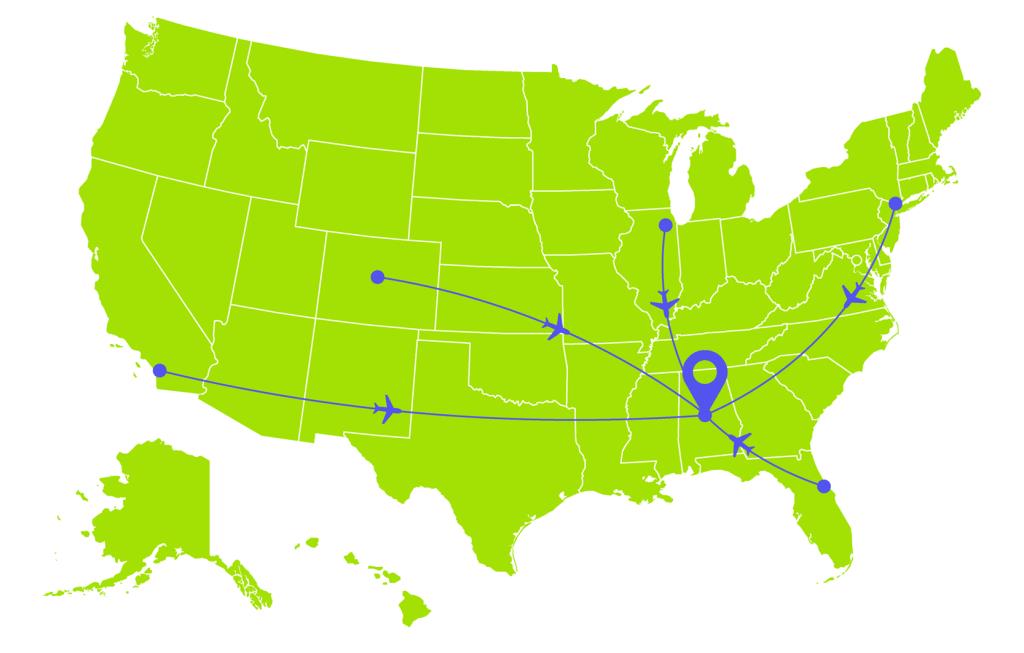
In 2022, Alabama arbitrarily reinstated an annual in-person visit requirement for patients with OUD. With no clinicians living in the state, tele-MOUD companies quickly stopped accepting new patients and eventually had to fly physicians to the state to see patients in-person, so those patients could stay in treatment. A year later, Michigan erected enormous barriers to tele-MOUD services for low-income patients on Medicaid. A legislature that prevents its most vulnerable citizens from accessing affordable, convenient and effective healthcare, should question its priorities and face the wrath of voters.
The Uncertain Future of Virtual Care
Even though telehealth treatment for OUD was implemented out of necessity during the pandemic, there’s no doubt it works. According to one study of Medicaid data, initiating treatment of buprenorphine for OUD through telehealth—versus in-person—increased the likelihood of patient retention. And people living in care deserts were finally able to access treatment for OUD perhaps for the first time thanks to telehealth expansion during COVID-19.
As of a few weeks ago, the Drug Enforcement Administration (DEA) has decided to temporarily extend COVID-era telehealth prescribing flexibilities through the end of 2024. While this is a sign that pleas from patients and providers are being heard, it’s still only temporary. What happens after 2024? What happens when states enact their own, stricter policies?
Accepting telehealth as a viable form of OUD treatment at the state and federal levels not just for now, but for the future, is an imperative and courageous step policymakers must take in order to quell growing OUD statistics.
In recent weeks, a bipartisan group of Senators re-introduced a bill (The TREATS Act which was initially introduced in 2020) which will increase access to telehealth services for OUD, effectively keeping the COVID-era regulations in place. There is no medical evidence to support the requirement for an in-person exam for OUD because a clinician is not required to physically examine a patient in order to make that diagnosis.
Courage begins with the willingness to listen and to reason. The DEA and the law makers behind the TREATS Act have exhibited that. After a major backlash to the DEA’s proposed rules released in February, they’ve taken a reasoned, courageous approach to updating the regulatory environment that is in the best interests of patient care.
The overdose crisis is a complex problem, but it is one that we can solve. We need to summon the courage to take action. We need to invest in new and innovative models for providing medication-assisted treatment. And we need to urge the DEA and Congress to make it easier for people to get the treatment they need. Ryan Hampton is an addiction recovery advocate and person in recovery. He was previously an official in the Clinton AdministrationHis most recent book is Unsettled: How the Purdue Pharma Bankruptcy Failed the Victims of the American Overdose Crisis












